Conditions
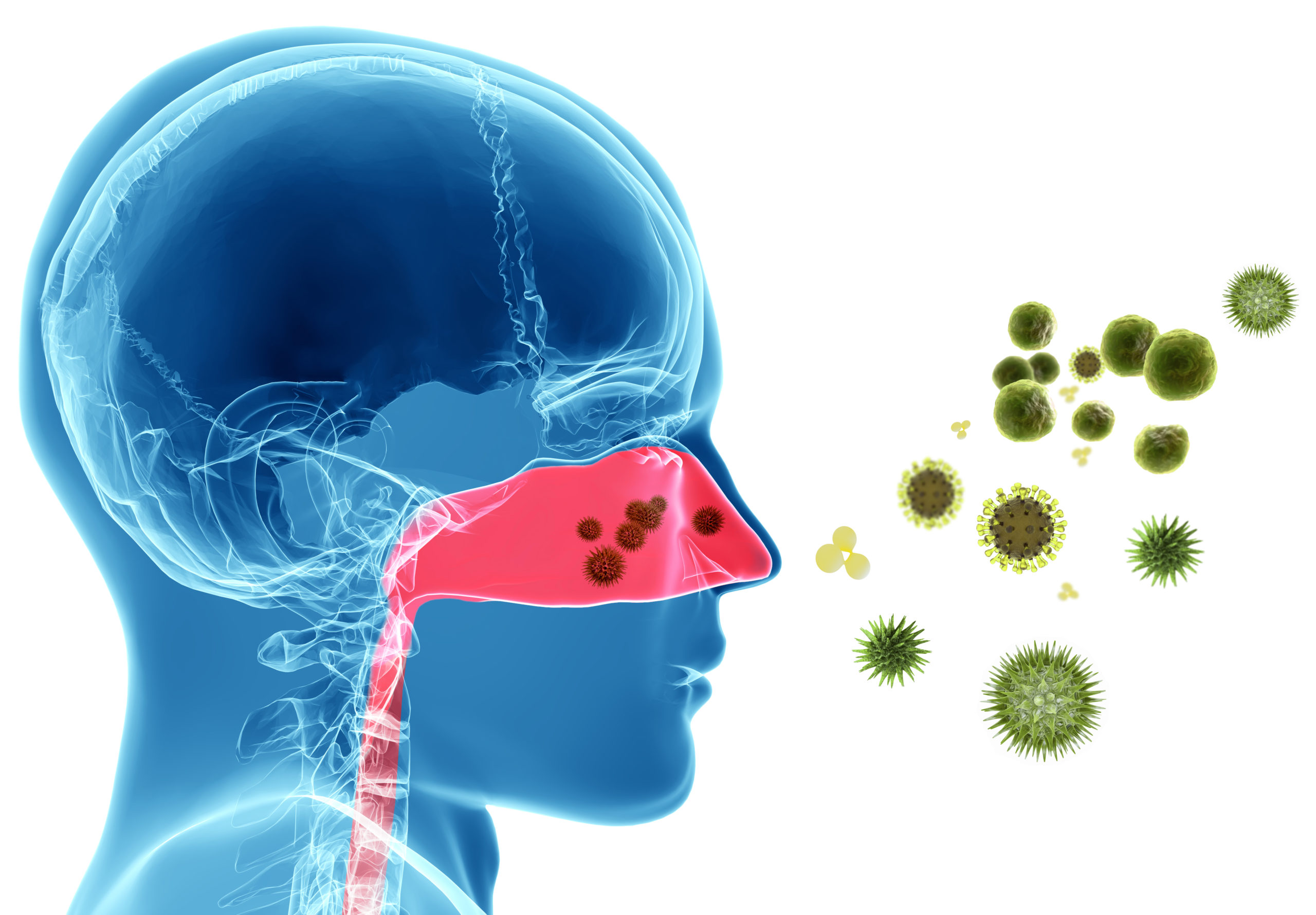
Allergic Asthma: 60% of all asthma is defined as allergic asthma. This subtype is defined by asthma symptoms that are triggered by allergens which include pollens, dust mites, cockroaches, and animal dander. These allergens cause inflammation leading to irritability and closing of the airways.
- Symptoms: Coughing, wheezing, shortness of breath and chest tightness.
- Diagnosis: In order to differentiate between allergic and non-allergic asthma, conducting allergy skin testing helps determine the specific allergens causing symptoms.
Treatments: Alongside using inhalers such as short-acting bronchodilators (rescue inhalers), inhaled corticosteroids, long-acting corticosteroids, and oral corticosteroids, our physicians specialize in providing long-term treatments that give increased relief. Allergen immunotherapy is most effective in desensitizing patients to improve their body’s immune response. Most recently, cutting-edge therapies such as biologics treatments like Xolair target specific cells involved in asthma, which is especially effective for patients with moderate to severe asthma. Biologics have been approved for children as young as 12 and all adults.

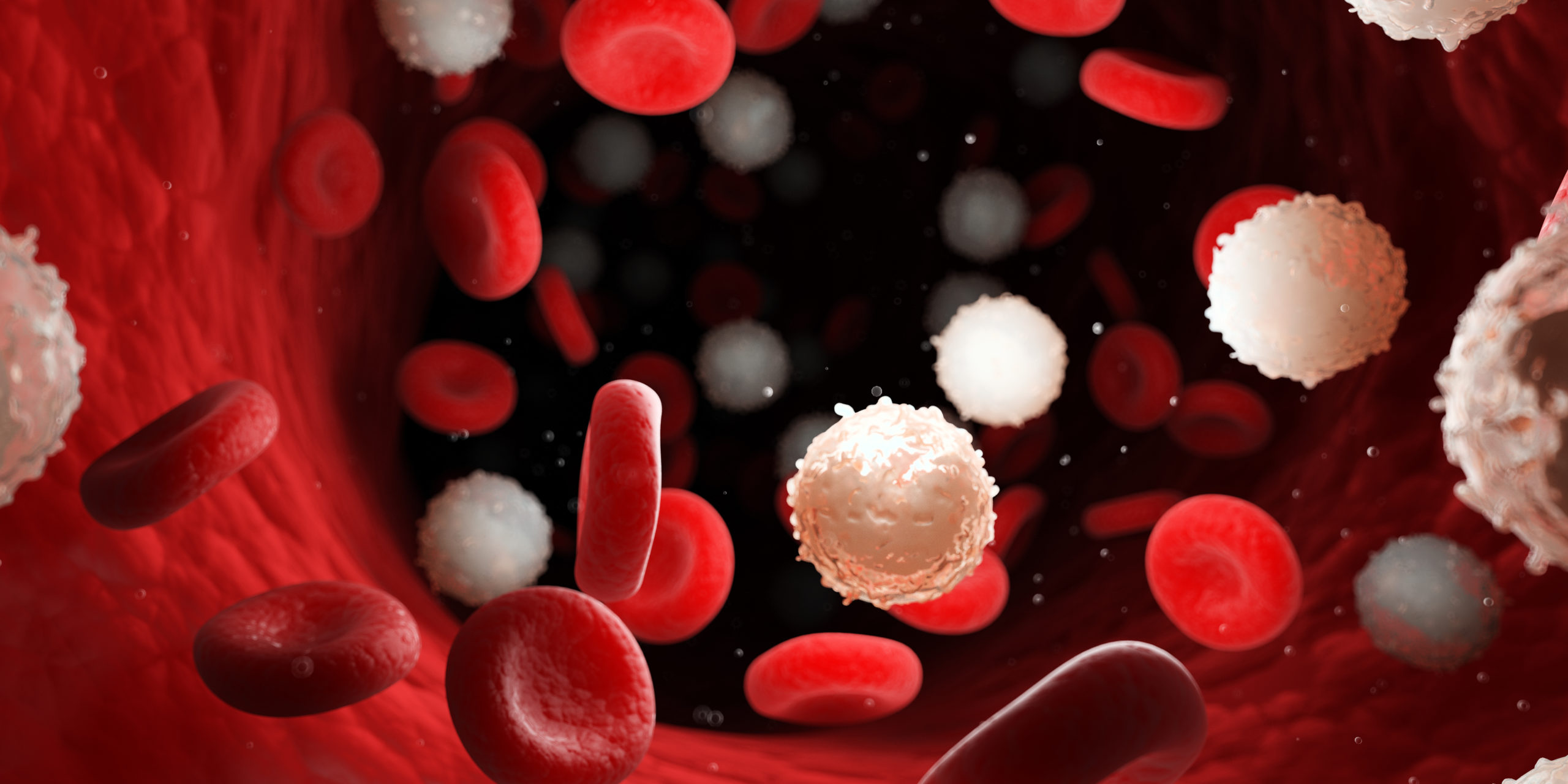
Eosinophilic asthma: Eosinophilic asthma is a subtype of severe, chronic asthma and is defined by the increased number of eosinophils (a type of white blood cell) in blood and tissue. This type of asthma primarily occurs in adulthood especially for those who are between 35-50 but has also impacted children. The two primary subtypes of Eosinophilic asthma are Atopic and Non-Atopic. Non-Atopic Eosinophilic Asthma, which is more common in severe cases in adults, involves innate immune pathways, whereas Atopic Eosinophilic Asthma is triggered by outside allergens and commonly overlaps with symptoms of allergic rhinosinusitis.
- Symptoms: Coughing, wheezing, shortness of breath, chest tightness. If patients have chronic sinusitis then they will also experience nasal congestion and sinus pressure.
- Diagnosis: The number of eosinophils is assessed in a blood sample or sputum sample (mucous that is coughed up). The results of these non-invasive procedures paired with clinical symptoms, and an Exhaled Nitric Oxide Test, which determines the amount of exhaled nitric oxide gas in a sample of a patient’s breath to assess the level of inflammation in your air passages, provide thorough evidence for an accurate diagnosis.
Treatments: Eosinophilic asthma is primarily treated with a combination of inhaled or oral corticosteroids/bronchodilators and biologics. Biologics are a class of advanced drug therapy that often have to be administered via injections in a medical setting. Examples include:
- Fasenra
- Dupixent
- Nucala
- Cinqair
By properly assessing your symptoms, health history, and breathing tests, our physicians are able to better determine which combination of asthma inhalers is best suited for you and your lifestyle. Though inhalers are common, the right inhaler or combination of inhalers is more difficult to prescribe. Inhalers fall into 6 main categories: Short and Long-Acting Bronchodilators, Short and Long-acting muscarinic antagonists, Inhaled Corticosteroids, and a Combination of inhaled steroids and bronchodilators. Along with ensuring the correct class of inhalers is considered, our team will be sure to give you a demonstration of how each inhaler should be used and properly cared for.

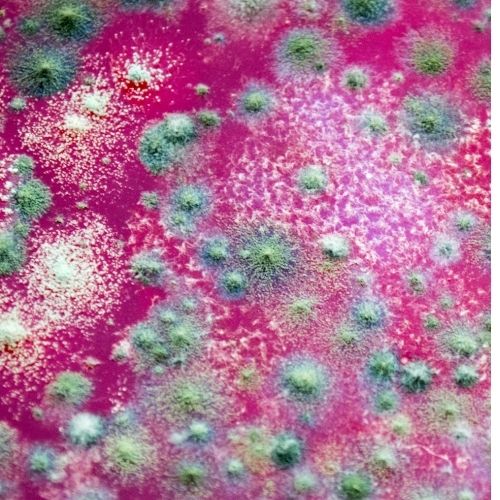
ABPA: Allergic Bronchopulmonary Aspergillosis is an allergic hypersensitivity reaction to fungus called Aspergillus Fumigatus. The fungus can cause an infection in the lungs and result in colonization of the airways. ABPA can cause worsening asthma, and people with Cystic Fibrosis are more susceptible to ABPA.
- Symptoms: Progressive or worsening asthma symptoms such as wheezing or shortness of breath, coughing with brown or bloody mucus, fever, or fatigue.
- Diagnosis: The most effective method to diagnose ABPA is through a combination of a medical history, skin testing and blood test to aspergillus fumigatus.
Treatments: Oral corticosteroids help open the airways to prevent the asthma symptoms associated with ABPA. Anti-fungal medications such as itraconazole can also be prescribed. Newer, off-label treatments include Xolair, a biologic treatment for severe, allergic asthma, has proven effective for some cases of ABPA.
AERD: Aspirin Exacerbated Respiratory Disease is an inflammatory disorder caused by an allergic reaction to aspirin and other Non-Steroidal Anti-Inflammatory Drugs such as ibuprofen and naproxen. AERD is often defined by nasal polyps, asthma, and chronic sinusitis.
- Symptoms: nasal congestion, runny nose, watery eyes, flushing of head and neck, coughing, wheezing, shortness of breath, chest tightness
- Diagnosis: The triad of defined characteristics along with clinical indication or the history of aspirin sensitivity supports diagnosis. Our physicians will also conduct a formal aspirin challenge to confirm diagnosis.
Treatments: Aspirin desensitization procedure conducted in a hospital setting is the most effective treatment for AERD, which also allows the patient to consume aspirin and NSAIDs without continued symptoms. Otherwise, patients are encouraged to avoid NSAIDs and take steroid treatments if needed. Recently, Dupixent, a biologic used to treat eczema, eosinophilic asthma, and nasal polyps, has been shown to be beneficial for AERD.

Intrinsic Asthma: Intrinsic Asthma is different from allergic, or extrinsic asthma, as it is triggered by conditions like weather, exercise, infections, and stress along with underlying genetics. In some cases Intrinsic Asthma has no known cause.
- Symptoms: coughing, wheezing, shortness of breath, chest tightness
- Diagnosis: a negative skin prick test and negative blood test combined with thorough patient history helps narrow down the diagnosis by eliminating the possibility of usual external allergens as causes.
Treatments: Along with identifying and reducing triggers that may cause intrinsic asthma symptoms the use of inhalers like other subtypes of asthma are standard. In addition, other effective treatments include oral medications such as Zileuton which block neutrophils (specific white blood cells), which are prominent in intrinsic asthma. Bronchial thermoplasty, which is a procedure upon which radiofrequency ablation of the thickened smooth muscle of the airways is done has shown to be effective. Immunosuppressive drugs such as methotrexate in some cases or the use of antibiotics in others has been proven to be effective as off label treatment.

Occupational Asthma: Caused by inhaling fumes, gases, dust, or other irritants while on the job. Examples include:
- Bakers: inhaling flour or baking enzymes
- Veterinarians/fisherman/Animal handlers- allergic reaction to animal proteins
- Healthcare workers: breathing in powdered proteins from latex gloves or mixing powdered medications.
- Symptoms: coughing, wheezing, shortness of breath, chest tightness
- Diagnosis: By a specialist obtaining a detailed history and identifying potential triggers.
Treatment: Avoidance measures to an offending agent is the mainstay of treatment.

COPD: Chronic obstructive pulmonary disease, represents a group of diseases defined by chronic inflammation of the lungs resulting in irreversible airflow obstruction. Chronic Bronchitis, Bronchiectasis, and Emphysema are the most common conditions that impact COPD. Smokers are most at-risk for developing COPD along with people who have had long-term exposure to toxic gases or particulates. In a small population of patients, COPD is a result of Alpha-1-antitrypsin deficiency, a genetic disorder where a decreased production of alpha-1-antitrypsin leaves the lungs unprotected and more vulnerable to long-term lung damage.
- Symptoms: COPD symptoms often arise after severe lung damage has happened and worsens over time. Symptoms are characterized by chronic, mucus-producing cough, respiratory infections, shortness of breath, chest tightness, wheezing, significant weight loss and loss of energy.
- Diagnosis: alongside a thorough health and family medical history along with potential exposures, our physicians will conduct spirometry tests to help determine lung function and irreversible obstruction. Chest x-rays/CT chest help rule out other lung problems or signs of heart failure, while highlighting diagnoses like emphysema. Alpha-1-antitrypsin deficiency lab tests, which is as simple as a small finger prick, can be conducted to test for the genetic disorder.

Asthma-COPD Overlap Syndrome- Condition whereby patients have both COPD and Asthma
Symptoms:
- cough,
- wheezing,
- shortness of breath,
- chest tightness
Diagnosis: a combination of a thorough medical history, imaging, and lung function testing will help in diagnosis.
Treatment: Standard treatment for both asthma and COPD includes the use of maintenance inhalers (e.g. inhaled steroids, long-acting muscarinic antagonists, long-acting bronchodilators, combination inhalers, and rescue inhalers. Biologics and allergen Immunotherapy is of consideration based on the subtype of asthma. Smoking cessation is also advised.

A chronic cough distinguishes itself from a normal cough related to asthma exacerbation or short-term viral or flu symptoms by the duration it lasts. In most cases, a chronic cough can last more than eight weeks in adults and more than six weeks. In most cases, chronic cough can impair daily functioning by disturbing sleep, causing exhaustion, impairing an active lifestyle, or making it difficult to carry a conversation. The top three causes of chronic cough are Laryngopharyngeal reflux (LPR) whereby stomach acid travels up to the esophagus and spills into the throat, allergic or non-allergic rhinitis defined by seasonal or environmental allergy symptoms and lower respiratory issues such as asthma or COPD exacerbation.
Symptoms:
- cough (in some cases mucus-producing and in rare cases producing blood),
- wheezing,
- shortness of breath,
- postnasal drip,
- sore throat,
- heartburn or acid reflux,
- runny nose,
- congestion
Diagnosis: a proper medical history in addition to a physical exam is very important to ascertain the possible causes. Procedures that may be needed are spirometry tests, upper endoscopy (from gastroenterology), rhino laryngoscopy (from ENT), skin prick testing to environmental allergens.

Treatments: Identifying the cause of chronic cough is the most effective way to ensure the right course of treatment is taken. For cases like GERD and laryngopharyngeal reflux, antacids such as H2 blockers, and Proton Pump Inhibitors paired with dietary or lifestyle changes are the most effective method of stopping chronic cough. For allergic or chronic rhinitis, a combination of antihistamines, nasal sprays, nasal irrigation, and allergen immunotherapy may help. For asthma, an improved inhaler regimen can be the answer to stopping the cough.
Chronic Pruritus: Pruritus is an itchy, irritated, or uncomfortable sensation on the skin that can progress and become persistent through time. It can be a result of a wide variety of causes, some that result from natural wear and tear, and others that are allergy-related. In some cases, a natural thinning of the skin in older patients leads to dryness in skin and itching. In other cases, irritation or allergic reactions from environmental or pollen allergens, contact allergens such as clothes, medications, or cosmetics, can result in eczema, hives, rashes, or other skin conditions that cause chronic pruritus. Nerve disorders in diabetic patients or people with multiple sclerosis can also cause a constant itching sensation, and the same goes for certain systemic conditions such as lymphoma, liver disease, or kidney failure. Psychiatric disorders such as anxiety or obsessive-compulsive disorder can cause chronic pruritus. We have also come to find that sensory receptors are also involved as part of the itching cycle.
- Symptoms: redness, bumps, cracked skin, dry skin, itching
- Diagnosis: skin prick testing to environmental allergens or patch testing to chemicals is the most effective way to determine an allergy-associated cause of the itchiness. To identify other causes, blood tests will be necessary to determine systemic conditions, and a detailed history to evaluate for any psychiatric conditions that may contribute.

Urticaria: Chronic Urticaria, or chronic hives, is characterized by itchy, red bumps or flat welts that vary in size, consistency, and appearance as a result of increased histamine release. Hives are considered chronic when they appear for more than six weeks or happen recurrently over the course of months or years. Urticaria can be separated into 5 major categories: Physical Urticaria, Autoimmune Urticaria, Allergic Urticaria, Idiopathic Urticaria and Urticaria associated with systemic conditions.
- Physical urticaria can be caused by dermatographism (welts or bumps that appear after scratching skin), pressure-induced, cholinergic (due to increase in core body temperature) heat or cold urticaria (eg. cold air, ice exposure, hot weather or hot drink exposure), solar (e.g. sun), aquagenic (e.g. water).
- Autoimmune urticaria: Patient develops an anti-IgE antibody that causes overt histamine release
- Allergic urticaria is a result of chemicals, environmental allergens, or foods.
- Idiopathic urticaria: Most common cause of chronic urticaria. Diagnosis of exclusion. Means that there is no known found cause of chronic urticaria.
- Urticaria associated with Systemic Conditions: There are associations with hypothyroidism with elevated thyroid antibodies, chronic infections, cancer, autoimmune disorders, Pan-hypogammaglobulinemia, parasitic infections, etc.
- Symptoms: red or skin-colored flat or raised welts, itching, swelling, sometimes associated with coughing, sneezing, shortness of breath, runny nose.

- Diagnosis: A thorough medical history is important. In addition, tracking a patient’s daily dietary habits as where the hives appear are crucial to help understand what potential triggers could be. After better narrowing those causes, our doctors can conduct skin-prick testing or patch testing to tease out allergens. Ice cube test can be done to diagnose cold induced urticaria.
Treatments: In addition to antihistamines, leukotriene antagonists, and potentially allergen immunotherapy, biologic drugs such as Xolair can be used for recalcitrant cases. Avoidance measures can also be implemented.
Dermatitis: Dermatitis is the general term for irritated, itchy, dry, swollen, or red skin. There are different types of dermatitis that are diagnosed, treated, and distinguished based on their causes.
Atopic Dermatitis is better known as allergic eczema and is caused by a specific allergen that often coincides with other allergy-related symptoms, but a family history of eczema can also be a risk factor and impact how severe the symptoms may be. Environmental allergens and especially in cases for children, food allergens can be provoking factors.
- Symptoms: dry, itchy, red, or irritated skin, raised bumps, red or brown patches of skin, swelling.
- Diagnosis: environmental and food allergen skin prick testing helps pinpoint the offending allergen. Intradermal skin testing is conducted for even more specific, sensitive identification of environmental allergens. For children, food challenges can be done in-office to determine if larger, underlying food allergies may cause eczema flare-ups.
Treatments: Alongside food and allergen avoidance, our physicians create a thorough eczema care plan which includes a combination of wet wrap therapy, moisturization, topical medications, and allergen immunotherapy. For patients with moderate to severe atopic dermatitis, including children as young as 6, Dupixent is a biologic injection that targets the underlying causes of inflammation and improves the quality of life.

Contact Dermatitis is characterized by redness, itchiness, and rashes as a direct reaction to chemicals (e.g. cosmetics, metals, medications, or fragrances).
- Symptoms: rash, dry, itchy, red, or irritated skin, swelling, bumps, blisters, or burning
- Diagnosis: our physicians have curated a comprehensive patch testing panel to test for some of the most common chemicals including metals and ones found in cosmetics. We employ chemicals suggested by the North American Contact Dermatitis Society in addition to much more.
Treatments: after identifying the specific allergens that have caused the reactions, we provide our patients with a thorough guide of products that do contain chemicals that can be avoided and alternatives to those products so you can continue to maintain their quality of life. Steroidal and nonsteroidal topical creams and antihistamines also help reduce the severity of symptoms until they are resolved.

Intrinsic Dermatitis is defined by the same symptoms as atopic dermatitis; however, intrinsic dermatitis is categorized as non-allergic. It often has a later onset, with milder symptoms, since these patients don’t have the Filaggrin gene mutation that is often seen in extrinsic dermatitis patients and causes skin barrier issues that are impacted by humidity and skin irritants. However, intrinsic dermatitis is characterized by a lower expression of interleukins and higher expressions of interferon-gamma. For some infants, these differences may be reflected by a change in gut flora that increases the risk of eczema.
- Diagnosis: blood tests that identify the amount of total IgE and specific IgE to specific allergens help determine the difference between intrinsic vs. extrinsic atopic dermatitis. Identifying triggers such as environmental and food allergens from skin prick testing is similarly important for intrinsic dermatitis.

- Symptoms: localized or generalized swelling, especially of the face, lips, tongue, throat, and eyes, redness, itchiness, or pain and warmth in affected areas.
- Diagnosis: health history alongside a family history and blood tests helps determine whether the swelling is histaminergic-mediated or bradykinin-mediated. Skin-prick testing helps pinpoint the allergen that may be associated. Treatments: preventive measures, antihistamines, leukotriene antagonists, allergen immunotherapy, Xolair are effective therapies for histaminergic-mediated angioedema. For bradykinin-mediated angioedema that may not be as receptive to these drugs. There are effective treatments for hereditary angioedema. For autoimmune or acquired angioedema, treating the underlying condition may help with attacks. Immunoglobulin-replacement therapy has also been shown to be a successful treatment for certain types of recurring bradykinin-mediated angioedema.

- Wheat-dependent exercise-induced anaphylaxis (WDEIA) is a severe food allergy that results in anaphylaxis 1 to 4 hours after wheat has been consumed and was followed by physical exercise. Aspirin, alcohol intake, infection, or stress can also take the place of exercise to insight the same reaction after wheat consumption.
- Idiopathic Anaphylaxis is a recurring, rare form of anaphylaxis with no identifiable triggers despite diagnostic assessments but happens to be more common in women than men. The diagnosis should only be made after thorough exclusion of other potential triggers.
- Alpha-Gal Syndrome starts with a Lone Star tick bite that transmits the alpha-gal molecule to a person. This molecule causes an immune response that results in anaphylaxis and similar allergic reactions to red meat or mammal products. The condition is primarily limited to the United States because of the tick’s presence here
- Symptoms: throat closure, throat swelling, throat pain, difficulty breathing, tongue swelling, shortness of breath, coughing, wheezing, low blood pressure, dizziness, fainting, fatigue, nausea, vomiting, diarrhea, congestion, runny nose, eye swelling.
- Diagnosis: After a thorough medical history and recounting instances of anaphylaxis, our physicians can determine which allergen testing would be most beneficial

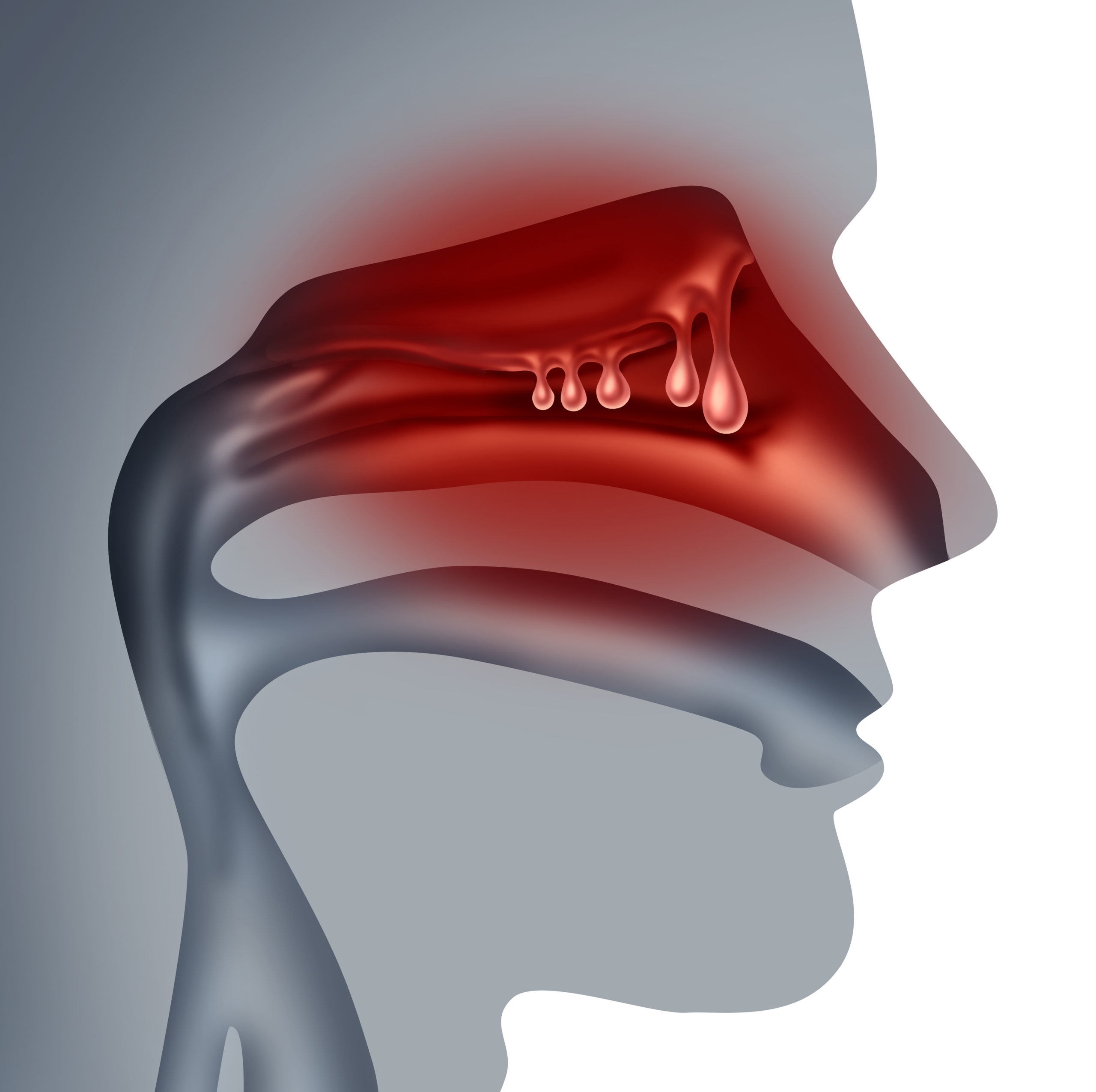
Chronic Sinusitis: chronic sinusitis is overt inflammation and infection of the sinus spaces located on face and forehead for three months or longer. The most common cause is due to uncontrolled inflammation caused by allergic and/or non-allergic triggers.
- Symptoms: redness, pressure, inflammation, pain, mucus discharge, postnasal drip, loss of smell or taste, ear pain, or fatigue.
- Diagnosis: CT of the sinuses helps identify which sinus cavities are affected. Obtaining a nasal culture can also be revealing in determining if there is an underlying infection. Skin-prick testing is a helpful determinant of what allergens could be causing the inflammation.
Treatments: use of intranasal sprays (e.g. antihistamine, corticosteroid. saline nasal irrigation, oral antihistamines, and antibiotics. Allergen immunotherapy is initiated for allergic causes to minimize future infections. A primary immunological evaluation is initiated and if an underlying immune deficiency is found, treatment will help minimize recurrent infections as well.

Nasal Polyposis: Nasal polyposis often coincides with symptoms of chronic sinusitis or chronic allergic vs non-allergic rhinitis. It is defined by small, non-cancerous, painless growths that are a result of chronic inflammation in the nasal passages and sinuses. These polyps can obstruct breathing and block nasal passages, but with treatment can reduce in size and frequency. The inflammation that causes these polyps are primarily a result of uncontrolled inflammation caused by allergic or non-allergic triggers.
- Symptoms: congestion, postnasal drip, runny nose, snoring, pain or pressure in the sinuses and around the face, loss of smell and taste.
- Diagnosis: a nasal endoscopy helps provide deep images to examine these polyps. CT scans can also help identify locations of polyps alongside sinusitis and other forms of inflammation. Allergen testing can tease out if allergens are triggering formation of these polyps.
Treatments: An aggressive nasal regimen of nasal corticosteroids and saline nasal irrigation can be extremely beneficial. Furthermore, allergen immunotherapy can minimize the development of polyps. Most recently, the FDA has approved Dupixent as a biologic injection treatment for the long-term resolution of nasal polyps, and other similar treatments like Nucala, Fasenra, and Cinqair have been indicated in providing significant improvement under clinical trials.
Allergic and Non-allergic rhinitis: Allergic rhinitis is what we identify as nasal inflammation provoked by allergens which we commonly refer to as hay fever. Some forms of allergic rhinitis are seasonal, such as symptoms caused by pollens, but others are perennial allergens such as animal dander, or dust mites can be year-round. Non-allergic rhinitis is inflammation provoked by irritants such as cold air, pollution, dust, wind, smell of fumes, or infection as opposed to allergens. It is important to treat both allergic or non-allergic rhinitis so upper airway inflammation does not trickle down to lower airways and cause development of asthma.
- Symptoms: sneezing, runny nose, postnasal drip, congestion, itchy or watery eyes, itchy nose, itchy throat, or fatigue
- Diagnosis: we are able to determine if a patient has allergic vs non-allergic rhinitis through allergy testing. While one may obtain blood tests, the most effective and sensitive testing is done through skin prick or intradermal testing.
Treatments: intranasal corticosteroids, anti-histamines, anti-cholinergic sprays are all effective therapy; however, our physicians specialize in providing long-term solutions to create effective change. The primary therapies that provide that long term relief are allergen immunotherapy that are either administered sublingually or subcutaneously (e.g. allergy shots).

Eustachian Tube Dysfunction: Eustachian tube dysfunction is typically pressure or irritation in your eustachian tube, the passageway between your middle ear that leads to your throat and nasal canal. The most common cause of this is inflammation or mucus build-up in the eustachian tube. Individuals who have persistent nasal inflammation are at increased risk of developing this (e.g., allergic vs non-allergic rhinitis). Overt nasal inflammation can be triggered by environmental allergens or irritants and infection. In addition, smoking may also contribute to mucus buildup from hurting the cilia in your ears, and even from obesity due to fatty deposits around your eustachian tube.
- Symptoms: fullness or popping in your ears, muffled sounds, ear or throat pain, ear ringing (tinnitus), issues maintaining your balance
- Diagnosis: our doctors will conduct a thorough examination of ear canals, ear drums, nasal and throat passages to determine eustachian tube dysfunction

Vocal Cord Dysfunction: Vocal Cord Dysfunction (VCD) happens when the vocal cords do not open correctly, resulting in breathing difficulties. VCD can often be mistaken for asthma due to the similarity in symptoms; however, many people with asthma can also have VCD. VCD happens more commonly in young, anxious, or athletic individuals.
- Symptoms: coughing, wheezing, shortness of breath, throat tightness, hoarseness of voice, difficulty talking.
- Diagnosis: Spirometry testing alongside a medical history helps differentiate out between asthma and VCD. A rhinolaryngoscopy will help better visualize the vocal cord and at times be able to capture any abnormalities of the vocal cord.
Treatments: Speech therapy and breathing techniques often help resolve vocal cord dysfunction. In cases whereby there is a mixed picture of asthma, a consistent regiment of inhalers is also important to provide overall care.

Drug Allergy: drug allergies are defined by four different types of hypersensitivity reactions whereby one’s immune system is having an overt reaction to a medication by misidentifying it as foreign and harmful. This is similar to the food and pollen allergy reactions we have. In some cases, allergies to drugs may not occur until several exposures to it. Some drugs commonly associated with allergies include antibiotics like penicillin, pain relievers such as non-steroidal anti-inflammatory drugs (NSAIDs), chemotherapeutic, and immunosuppressants.
- Symptoms: hives, throat swelling, tongue swelling, difficulty breathing, coughing, wheezing, shortness of breath, rashes, runny nose, itchy or watery eyes, anaphylaxis
- Diagnosis: our physicians specialize in providing in-clinic drug skin testing. If skin testing is noted to be negative then a drug challenge may be pursued where the patient is given small, increasing amounts of the drug that may be causing the reaction to see if this is a true allergy.
Treatments: for a certain type of drug allergy a desensitization procedure may be pursued. This is a process whereby small, increasing amounts of the medication may be given to get your immune system used to it so an individual may complete a course of treatment without getting an allergic reaction. Aspirin desensitization is a common therapy that helps patients who have allergies to aspirin to be able to take this medication. This is especially beneficial for patients who also need to take aspirin for cardiac issues.

Venom Allergy: Venom allergies are primarily associated with reactions after a sting from a bee, wasp, yellow jacket or hornet sting.
- Symptoms: itching, hives, swelling of the tongue, throat, or lips, throat closure (consistent with anaphylaxis), difficulty breathing, stomach pain, nausea, vomiting, or diarrhea
- Diagnosis: We offer several different methods of testing for venom allergies, which include a blood test, skin prick and intradermal testing, common venoms such as honeybee, wasp, yellow jacket, white-faced hornet and yellow-faced hornet.
Treatments: One may decrease the risk of getting stung by not disturbing nets of bees, wasps, yellowjackets, or hornets. Also, it is recommended to avoid bright clothing or wearing perfume in areas that may have more of these insects. Our providers also offer venom immunotherapy, that helps provide long-term resolution of future anaphylaxis or allergy reactions to stings. Similar to our environmental allergen immunotherapy, patients are given small increasing doses of venom as a way of allowing the immune system to become tolerant to the venom allergen to minimize severe allergic reactions.

Skeeter Syndrome: Skeeter syndrome results in a larger or worse localized reaction to a mosquito bite, which can often be mistaken as an infection or a result of scratching the affected area. However, the syndrome is an allergic reaction to the protein in mosquito saliva.
- Symptoms: red, itchy bumps, swelling, hives, warmth or pain in affected area
- Diagnosis: health history and description of identification of the localized reaction
Treatments: supportive care is the best method to relieve symptoms associated with Skeeter syndrome. This includes cold compress on the affected area, calamine lotion, corticosteroid creams, anti-inflammatory creams or ointments, and oral antihistamines.

Allergic reactions to vaccines are often caused by the vaccine components rather than the actual immunizing agent itself. Common allergen vaccine components include egg, latex, gelatin, yeast, neomycin, and thimerosal.
- Symptoms: local or generalized swelling, red, itchy bumps where the vaccine was administered, coughing, wheezing, shortness of breath, throat tightness.
- Diagnosis: after looking at the components of the vaccine that was administered, we can effectively test for a reaction to the specific allergen component that may be the cause of the adverse reactions. This can be done through skin prick testing to egg and yeast, or patch testing to latex, neomycin, latex, thimerosal or other chemical components.
Treatments: Though vaccine allergies are very rare, in the case you test positive to a component of the vaccine, in most cases you can find alternate vaccines that do not have those components. Other options include taking corticosteroids or antihistamines prior to vaccine administration depending on the severity of the reaction.

Food Allergy: The three main types of food allergies are Immunoglobulin E (IgE) mediated, non-IgE mediated, and mixture of IgE + non-IgE mediated. IgE-mediated food allergies are ones that occur within seconds to 2 hours that commonly cause urticaria (hives) , angioedema (swelling), and anaphylaxis (throat tightness, vomiting, decrease in blood pressure). Non-IgE-mediated reactions are more difficult to diagnose and often happen several hours after food consumption, making it hard to pinpoint the trigger (e.g. Food protein induced enterocolitis). Mixed IgE + non-IgE food allergies have symptoms of both the immediate onset and late (e.g. eczema, eosinophilic esophagitis). Your body can have an allergic reaction to any food, but the most common food allergies come from milk, eggs, peanuts, tree nuts, fish, soy, wheat, and shellfish, especially among younger children.
- Symptoms: itchiness in the mouth, lip swelling, tongue swelling, throat swelling, coughing, wheezing, shortness of breath, difficulty swallowing, runny nose, sneezing, rash, itchiness, bumps, nausea, vomiting, stomach pain, dizziness, diarrhea,
- Diagnosis: understanding symptoms, when they occur, and the different foods that may be the culprit, paired with skin prick testing to food allergens is the most effective way to pinpoint the food trigger. Our physicians have a panel of over 80 different food allergens to test. Additionally, comprehensive blood tests with component testing can provide more insight. Food challenges, especially for children who have a higher chance of allergy to common allergens, provide helpful insight within a clinical setting to give your child the care they need.
Treatment:
In most cases, avoiding the food allergen is the best way to ensure symptoms do not arise. Many times patients will be prescribed an epi-pen to carry with them if they’ve had severe anaphylaxis reactions in the past. Our medical team provides patients with full training on how to use the epinephrine auto injector so in the chance they have to, you will feel comfortable and confident in doing so. We have also invested time in researching the most groundbreaking food allergy treatments. We offer oral immunotherapy (OIT) as a long-term solution for food allergies. OIT is a form of food allergy treatment that involves feeding an allergic individual with gradually increasing amounts of the target food allergen(s) over several months. The goal of this therapy is to raise the individual’s threshold that may trigger a reaction and provide them with protection against accidental ingestion of the allergen. This level of protection will improve the quality of life for both patients and their families by reducing the fear of accidental ingestion and life-threatening reactions. Recently, the FDA has approved Xolair, a biologic injection treatment to serve as monotherapy for food allergies in addition to the effective relief it has already provided for chronic urticaria and severe asthma.

Eosinophilic Esophagitis or EoE is chronic, allergic, inflammation of the esophagus that is caused by the accumulation of eosinophils, white blood cells that play a role in our body’s immune response. This is often characterized by food getting stuck in one’s throat. Patient’s who have EoE also commonly have allergic rhinitis and other conditions such as asthma and eczema.
- Symptoms: heartburn, difficulty swallowing, throat pain, food impaction, nausea, vomiting, weight loss or malnutrition, stomach pain, chest pain
- Diagnosis: Upper endoscopy with biopsy will help diagnose EoE along with the medical history obtained. Considering this is a IgE + non IgE reaction skin testing will prove to be beneficial to some patients.
Treatments: The most effective treatment for EoE is swallowing inhaled steroids (e.g. fluticasone propionate), or swallowing of budesonide oral suspension, which help coat the esophagus and control inflammation. Another form of treatment is avoidance of the offending foods. This can be done by implementing a four or six food elemental diet or determining the food by history or with skin testing. Currently Dupixent is in phase III trials for treatment of EoE that is showing promising results.
- Symptoms: stomach pain, fatigue, vomiting, nausea, weight loss
- Diagnosis: Upper endoscopy is also an effective way to diagnose EG by identifying irritation in the stomach lining; however, in many cases biopsies of the esophagus, stomach or small intestine are also necessary to make a sure diagnosis to clearly see the chronic inflammation and help rule out other gastrointestinal causes. Additionally, skin prick testing and blood tests are done to identify food triggers that may be exacerbating EG symptoms.
Treatment: It is important to avoid food allergens or triggers. Our doctors This can be done by implementing a four or six food elemental diet or determining the food by history or with skin testing. Short term oral steroids and viscous budesonide may be considered.

Food Protein-Induced Enterocolitis (FPIES): FPIES is a type of delayed type of food allergy (occurring any time after 2 hours of ingesting the food) that causes symptoms such as vomiting, diarrhea, blood tinged stools, dehydration, and failure to thrive. Considering the type of immune response that causes this reaction skin prick testing is not useful in determining the food allergen. However, commonly, foods such as soy, milk, rice, and grains are the major culprits.
- Symptoms: vomiting, diarrhea, bloody diarrhea, abdominal pain, loss of appetite, slow growth, malnutrition, rapid weight loss, low blood pressure, dizziness, fatigue
- Diagnosis: medical history is the most important clue to diagnosing. At times an oral food challenge may be necessary to diagnose the offending allergen.
Treatments: Avoidance of the food is the mainstay of treatment. It is most important to keep children hydrated and provide supportive treatment in case a reaction were to occur. Our physicians help parents create custom dietary plans to avoid the allergen while ensuring your child is still receiving the proper nutrition they deserve. Luckily, in most cases FPIES resolves on its own with time, good nutrition, and age.

Oral allergy syndrome (OAS): Oral allergy syndrome, also commonly referred to as Pollen Fruit Syndrome, is a food allergy caused as a result of cross-reactivity of proteins found in pollen with proteins found in certain raw fruits, vegetables, grains, and nuts. For the most part it causes itching of the mouth. In approximately 1% of cases this may lead to anaphylaxis.
- Symptoms: itchiness, redness, or swelling of the mouth, lips, tongue, and throat, difficulty breathing, difficulty swallowing
- Diagnosis: skin prick testing to our 80-allergen food panel has been effective in identifying the fruits, vegetables, nuts, and grains causing these symptoms. For higher sensitivity, our practice also conducts prick-prick testing to study the direct skin reaction from the fruit or vegetable in question.
Treatment: In 30-50% of patients, allergen immunotherapy to environmental allergens may help improve OAS symptoms. For most OAS cases, the allergen does not have to be fully avoided. Cooking or heating the particular food in question breaks down the protein and makes it less allergenic.

Latex Fruit Syndrome: Latex fruit syndrome is a fruit or vegetable allergy limited to people who already have latex allergies and happens to 30-50% of these patients. Proteins in latex cross-reaction with the proteins in these particular fruits and vegetables. The reaction can happen after eating, touching, or smelling these foods. Some of the highly latex cross-reactive foods include: avocado, bananas, chestnuts, kiwi, tomatoes, melons, papaya, celery, carrots, apples, and papayas.
- Symptoms: can be highly variable by may include urticaria ( hives), angioedema (swelling), and anaphylaxis severe allergic reaction leading to wheezing, shortness of breath, throat closure, low blood pressure)
- Diagnosis: food allergen skin-prick testing as well as prick-prick testing to specifically latex cross-reactive foods are most beneficial in identifying this allergy for patients who already suffer from latex allergies.
Treatments: Avoidance of foods that the patient had a reaction to and being mindful of the foods latex cross-reacts with is important.

Gluten Sensitivity: Gluten sensitivity is intolerance to gluten found in wheat, rye, and barley often characterized by stomach pain, muscle cramps, constipation, bloating, or diarrhea. This is distinct from Celiac disease which is an autoimmune response against the proteins in gluten that results in damage to the small intestine lining, resulting in long-term, and in some cases severe, damage. Celiac disease can also be distinguished from gluten intolerance by bloody diarrhea, weight loss, and at times a specific type of eczema noted on arms called dermatitis herpetiformis. “Gluten allergy” is an inaccurate designation as this condition does not exist. Individuals commonly have a reaction to wheat which may include urticaria, angioedema, or anaphylaxis.
- Symptoms: bloating, stomach pain, muscle cramps, constipation, bloating, diarrhea, weight loss, itchy skin, runny nose
- Diagnosis: first, a blood test will be done to ensure the symptoms are not associated with Celiac disease. Once that’s been ruled out, food allergen skin prick testing, specifically to wheat, rye, and barley gives an accurate distinction between a wheat allergy vs gluten intolerance.
Treatments: though avoiding gluten is helpful, a completely gluten-free diet is not recommended because of complexity and risk of nutrient deficiencies. Instead, our physicians can help come up with a manageable nutrition plan that provides alternatives to common wheat, barley and rye containing foods without having to dramatically change your lifestyle.

Lactose Intolerance: Lactose intolerance is an often acquired condition that happens to most people later in life and prevents the complete digestion of the sugar lactose in milk. The small intestine naturally produces the enzyme lactase which helps break down lactose. However, low levels of lactase production can make it more difficult to completely digest milk products, moving the lactose into the colon instead of it being processed and absorbed, resulting in stomach and gastrointestinal discomfort.
- Symptoms: bloating, gas, cramps, nausea, stomach pain, vomiting, diarrhea, loose stool
- Diagnosis: typically a medical history will suffice. A Lactose intolerance test can also be done which is a blood test done two hours after drinking milk to measure the amount of glucose in your bloodstream. Low amounts of glucose mean your body’s lactase enzymes haven’t properly broken down the lactose to glucose.
Treatments: Dairy avoidance is recommended along with taking Lactaid tablets prior to any meals containing dairy.

Primary & secondary Immunodeficiencies: Immunodeficiencies are disorders that fully or partially weaken the immune system, leaving our bodies more vulnerable to infections, cancers, and other health issues. Primary Immunodeficiencies are a result of genetic defects that impair the immune system. There are more than 150 primary immunodeficiencies diagnosed. In contrast, secondary immunodeficiencies are acquired as a result of treatments, infections, or illnesses that have weakened the body’s immune defense.
Primary Immunodeficiencies include but are not limited to:
- Common Variable Immunodeficiency (CVID)– due to a mutation in genes that impair the development and function of B cells that leads to a decrease in quantitative immunoglobulins (Ig) such as IgA, IgM, IgG in conjunction with a poor functional antibody response. People with CVID often develop pneumonia and acquire infections that specifically affect the lungs, sinuses and ears.
Hypogammaglobulinemia is an immune impairment where the body does not produce enough gamma globulins such as (e.g IgG) resulting in a decrease in antibody production. Secondary factors such as medications and poor nutrition can exacerbate or trigger the onset of Hypogammaglobulinemia.
Secondary immunodeficiencies include but are not limited to malignancies such as Lymphoma and Leukemia, HIV, Diabetes, burns, poor nutrition.
- Symptoms: individuals tend to have more frequent infections such as 3-4 sinus infections yearly, more severe infections taking longer time to treat, as well as infections requiring intravenous antibiotics. In conjunction, individuals may develop autoimmune, gastrointestinal, inflammatory, or underlying malignancies
- Diagnosis: via a combination of a thorough medical history along with blood tests. We are able to see via a blood test the quantity of immune cells and whether they work properly.
Treatments: Depending on the type of immune deficiency, patients may be a candidate for either prophylactic antibiotics, immunoglobulin replacement therapy, bone marrow transplant or just surveillance. Our providers understand the fear and anxiety that comes with immunodeficiencies and will work with patients to provide the most effective care.
Autoinflammatory disorders: Autoinflammatory conditions are disorders caused by genetic mutations that cause dysregulation of inflammatory mediators leading to recurrent fevers and organ damage.
- Symptoms: common symptoms in all autoinflammatory conditions include, fevers, rashes including urticaria, joint pains, arthritic pain, malaise, urticaria, vomiting, diarrhea, blood protein build up, swelling, enlarged lymph nodes, ulcers.
- Diagnosis: a combination of physical exam, health history, family health history, blood tests, and genetic testing provide an accurate diagnosis
Treatments: Treatments available include Anakinra (Kineret), canakinumab (Ilaris), and colchicine have been proven to have the most important and widespread positive impact on autoinflammatory disorders. Our doctors will work closely with the patient’s preferred rheumatologist to constantly monitor symptoms and provide support.

Familial Mediterranean Fever: an inherited disorder that primarily affects people from the Mediterranean region (North African, Arab, Armenian, Turkish, Greek, Jewish, Italian) that cause arthritic attacks from a young age along with fever, abdominal pain, chest pain, swollen joints, or red rashes.

Cryopyrin-Associated Periodic Syndromes (CAPS)– is a rare hereditary disorder encompassing a continuum of three phenotypes: familial cold autoinflammatory syndrome (FCAS), Muckle-Wells Syndrome (MWS), and neonatal-onset multisystem inflammatory disease (NOMID).
- Muckle-Wells Syndrome: the most common symptom of MWS is chronic, recurring, non-pruritic rashes that start in early infancy or childhood. The rashes and other symptoms of headaches, fevers, and joint pain can be triggered by cold, stress or other factors and can lead to progressive, significant hearing loss.
- Familial cold autoinflammatory syndrome (FCAS)- also known as familial cold urticaria, is a rare, inherited inflammatory disorder characterized by intermittent episodes of rash, fever, joint pain and other signs/symptoms of systemic inflammation triggered by exposure to cold.
- Neonatal onset multisystem inflammatory disease (NOMID)- is a disorder that causes persistent inflammation and tissue damage primarily affecting the nervous system, skin, and joints.
TNF-Receptor Associated Periodic Syndrome (TRAPS): this disorder is caused by the mutation in the TNFRSF1A gene that is inherited. TRAPS is defined by a rash that spreads over the body often with deep tissue pain, swelling of the eyes and redness of the eyes.

Hyper IgD Syndrome (HIDS): is also an inherited autosomal recessive disorder caused by the gene mutation in the mevalonate kinase gene. It is often diagnosed from continuously high IgD levels and symptoms appear within the first year of life, defined by quick rise in temperature that causes fevers for up to a week along with urticaria, headaches, joint pain, arthritis, enlarged lymph nodes, vomiting, diarrhea, or ulcers

Mast Cell Activation Syndrome (MCAS)/Mastocytosis : both are caused by a defect that leads to overactivation and degranulation of mast cells that results in release of mediators that lead to symptoms such as urticaria, angioedema, and at times anaphylaxis.
- Symptoms: urticaria, pruritus, angioedema, low blood pressure, redness, tachycardia, coughing, wheezing, shortness of breath, throat closure, difficulty breathing, diarrhea, nausea, vomiting, stomach pain
- Diagnosis: a thorough medical history in combination of blood, urine, and at times a bone marrow biopsy may be warranted.
Treatments: Commonly symptoms are treated or prevented by giving a regimen of anti-histamines, leukotriene antagonists (e..g montelukast), and on demand need for epinephrine may be needed for certain individuals. Recently, Xolair has been tested to provide long-term relief to MCAS patients because of its ability to reduce mast cell reactivity. Chemotherapeutic agents at times may be needed for severe forms of mastocytosis.
Hypereosinophilic Syndrome is a group of blood disorders that happens as a result of too many eosinophils (e.g. absolute count above 1500), a type of white blood cell, in your body. Eosinophils are produced as an immune response, but an overproduction can infiltrate various tissue and eventually damage organs
- Symptoms: fatigue, cough, shortness of breath, muscle pain, rash, and fever
- Diagnosis: After obtaining a thorough medical history our doctors can determine the proper blood tests to evaluate increased eosinophils paired with X-rays and CT scans of the chest and organs.
Treatments: The first course of treatment is typically systemic corticosteroids like prednisone to help decrease the eosinophil count to reduce organ damage. Nucala has also been approved for treatment.