Understanding your insurance benefits can be daunting, but is very important to staying informed on what you are responsible to pay. For that reason, we have created a list of the most common questions regarding insurances. Let’s get started!
What are the terms you need to know?
Your monthly premium is what you pay each month to keep your insurance active. In addition to your monthly premium, you may also have out-of-pocket costs, which is what you are responsible to pay when you require care.
Out-of-pocket pocket costs include:
- Deductible: what you must pay each year before your insurance begins paying.
- Copayment: what you pay to see a doctor. Your copay may be different to see your PCP and a specialist and is normally due at the time of your visit.
- Co-insurance: the percentage of your bill that you are responsible to pay.
- Out-0f-pocket maximum: the maximum amount that you can spend in a year. Typically, once your out-of-pocket maximum has been satisfied, you will be covered 100% for covered services.
It is important to know if your doctors are in-network or out-of-network.
- In-network means that your health plan has a contract with that provider. Out-of-pocket costs may still apply for in-network providers, but are typically less expensive than they are for out-of-network providers.
- Out-of-network means that your health plan does not have a contract with that provider. Out-of-pocket costs are typically more expensive than they are for in-network providers.
What are the different types of insurance plans?
- HMO plans require you to see doctors that are in its network. Most HMO plans require you to get a referral from your PCP in order to see a specialist. Once you begin seeing a specialist, you will need an authorization for each visit and service. Often, your specialist will submit these referrals in order to continue your care. If you decide to see a doctor that is out-of-network, your insurance company will normally not cover you, and you will be responsible to pay for 100% of the costs. Typically, your premium and out-of-pocket costs will be lower for HMO plans than PPO plans.
- PPO plans offer more flexibility when selecting a provider. You do not need to see your PCP before seeing a specialist or obtain referrals. Many PPO plans have both in-network and out-of-network benefits. Although, if you decide to see a doctor that is out-of-network, your out-of-pocket costs may be higher. Typically, premiums and out-of-pocket costs are higher for PPO plans than HMO plans.
- Medicare is a federal health insurance program for people who are 65 and older or for younger people who have specific disabilities. Medicare has different parts which offer different coverage and you may not have every part.
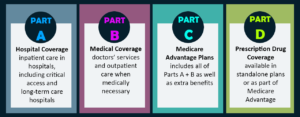 Part A: Is hospital insurance which covers inpatient hospital services.
Part A: Is hospital insurance which covers inpatient hospital services.
Part B: Is medical insurance which provides coverage to see certain doctors.
Part C: Is a Medicare Advantage Plan. This is a type of health plan that is contracted with Medicare to provide part A and B benefits. These plans may be PPO, HMO or other types of plans.
Part D: Is prescription drug coverage.
- Medi-Cal (or Medicaid) is the California Medical Assistance Program which offers insurance for low-income individuals. Our practice currently requires medi-cal patients to have an authorization in order to see us.
Who is responsible for confirming your benefits?
It is the patient’s responsibility to confirm and understand his or her benefits. Understanding your benefits is important to do before seeing a doctor so that you know what you are going to be responsible to pay. However, as your insurance provider will inform you, confirming your benefits is not a guarantee of payment. Despite this fact, the more informed you are, the less likely that you will be surprised when your bill comes in. You can confirm your benefits by calling the customer service phone number on the back of your insurance card.
