Eczema is a common skin condition that affects about 30% of the US population. It is characterized by dry, scaly patches on the skin that can be itchy and irritated. Eczema is more often diagnosed in childhood, but it can affect adults as well. Flare-ups of eczema tend to occur in the winter and summer months and can be triggered by changes in weather. Eczema has various subtypes, and it can be caused by a combination of allergies, diet, and genetic mutations. Learning more about the types and causes of eczema can better help us treat our patients!
What are the different types of eczema?
Atopic Dermatitis
The most common type of eczema is atopic dermatitis or “allergic” eczema. This type is generally diagnosed by testing positive on an allergy skin test to environmental allergens and having a high immunoglobulin E level in the blood. Allergy skin prick testing helps to determine common triggers such as dust mites, cat and dog dander, and pollens that may be provoking eczema flare ups.
Eczema is especially common in children, and approximately 10 to 20% of children are diagnosed. Atopic dermatitis is considered to be part of the “atopic march”. This means that a diagnosis of eczema could be accompanied by food allergy, allergic rhinitis, and asthma, in that order.
About 33 to 63 percent of young children with moderate to severe eczema also have food allergies. Therefore, it is important to bring children under the age of 5 to be evaluated by an allergist for milk, egg, peanut, wheat, and soy allergies even if they have not had past adverse reactions to these foods. A skin prick test to these foods of interest will allow your allergist to create a specific treatment plan that may involve eliminating some foods from your child’s diet.
Additionally, studies have shown that 80% of children with eczema develop allergic rhinitis and/or asthma later in childhood. This is why it is crucial to see your allergist at the first sign of eczema symptoms. If your child is experiencing flare ups, their eczema may need to be addressed through several different approaches. Your allergist will be able to conduct more comprehensive testing to evaluate whether allergic rhinitis and asthma may also be playing a role.
Intrinsic Dermatitis
Another type of eczema that is more uncommon is intrinsic eczema, which has not been found to have any association with allergies. This form is diagnosed when immunoglobulin E levels in the blood are normal and skin testing to environmental allergens is negative. In recent studies, the function of the skin barrier was better preserved in patients with intrinsic dermatitis compared to patients with atopic dermatitis (Kulthanan et al, 2011). The causes of intrinsic eczema are not well known but have been linked to an underlying genetic mutation in the FLG gene, which controls the expression of filaggrin, a protein found in our skin cells (Shobaili et al, 2016). Recent studies show that the FLG gene has an important role in maintaining skin barrier function and regulating the pH and hydration of our skin. If the gene is not functioning properly, allergens can enter the damaged skin barrier more easily, resulting in the skin inflammation and irritation (Kulthanan et al, 2011)
Some people may be born with FLG mutations while others may be more susceptible to developing them depending on their environment. Some factors that are have been correlated with FLG mutations are low humidity conditions, exposure to skin irritants, and age (Shobaili et al, 2016).
Additionally, intrinsic dermatitis may be influenced by our microbiome, or the composition of bacteria found on the surface of our skin and in our guts. Staphylococcus aureus is a type of bacteria that has been found in higher amounts in the skin microbiome of eczema patients during a flare-up (Pierce-Fisher 2017).
Gut bacteria also has a similar effect in inducing inflammation, and studies have shown a strong correlation between a bacteria called Faecalibacterium prausnitzii and intrinsic eczema (Lio and Lal) Additionally, there was a much lower diversity of gut bacteria found in infants with eczema compared to infants without (Zheng et al 2016). Finally, elimination diets and probiotics may be used to treat skin inflammation associated with the gut microbiome, but have been found most effective when used for prevention(Lio and Lal). Although not much is currently known about the association with the gut microbiome and eczema, future treatments that target specific gut bacteria are promising in improving symptoms!
Contact Dermatitis
The last type of eczema is caused by coming in contact with irritants ranging from common household chemicals to cosmetics and metals. This type of eczema occurs exclusively when our skin comes in contact with an irritant. The skin inflammation that occurs from exposure to an irritant may manifest immediately after or up to a week after contact. You may notice blisters, redness, and itching in specific areas that made contact with an irritant.
At our office, we use a 3 day procedure known as patch testing to evaluate triggers for contact dermatitis. This test consists of applying a patch of several chemicals to the back and reading any skin reactions that show up 48 and 72 hours after application. However, some reactions may present up to 5 or 7 days later. Contact dermatitis is managed primarily by avoiding the products that can trigger a reaction and flare ups are managed with topical ointment treatment recommended by your allergist.
So, what should you do if you or your child have eczema?
The good news is that there are several accessible and effective treatments to manage and treat eczema!
With atopic dermatitis, it is recommended that you or your child first have skin prick testing done to evaluate environmental and food triggers for flare ups. Skin care is a priority for managing eczema, and your allergist will develop an eczema action plan tailored to you, which will detail how to use different moisturizers and topical ointments to manage the varying severity of your flare ups. These ointments vary in potency and high potency ointments will be effective for more severe flare ups.
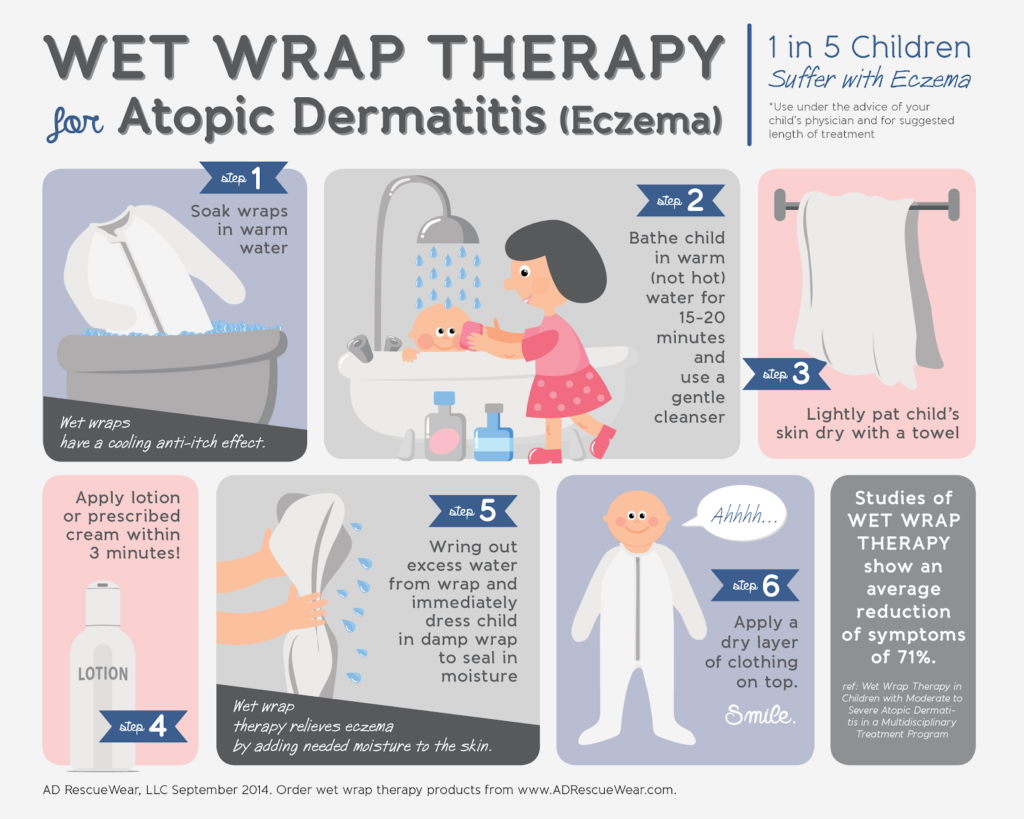
Additionally, a method known as wet to dry wrapping is a natural method that can help seal moisture within the skin, preventing dry and scaly patches. Wet wrapping is most effective after bathing, moisturizing, and applying medications.
While skin care is crucial, it is often accompanied by allergen immunotherapy, or allergy shots, to tackle the environmental allergens that trigger flare ups. Your allergist will develop a custom serum for you based on skin test results, and this sensitization process has been shown to reduce frequency of eczema flare ups.
If your child’s flare ups remain persistent despite an extensive skin care regimen, it is recommended they be tested for milk, egg, peanut, wheat, and soy allergies. Your allergist may recommend an elimination diet or avoidance of these foods along with a topical ointment regimen.
Finally, preventative measures can also be helpful in helping control the frequency and severity of flare ups. It is recommended that you use dust mite covers around mattresses and pillows, double wash sheets and blankets in warm water to kill bacteria, and keep indoor humidity low. In order to minimize animal dander triggers, avoid contact with pets or obtain a HEPA filter.
If you have severe eczema and experience persistent flare ups despite an aggressive skin care regimen and immunotherapy, you may be a candidate for a biologic medication called Dupixent. This treatment is self-injectable after the first dose. Please make an appointment so you can discuss all your available options with an allergist!
In summary, it is important to address these concerns sooner rather than later, as many eczema symptoms are also associated with underlying allergy and asthma diagnoses. Seeing your allergist to determine the best course of treatment for you will ensure that all your symptoms are properly addressed.
Sources:
https://acaai.org/allergies/types-allergies/skin-allergy/eczema-atopic-dermatitis
https://nationaleczema.org/atopic-dermatitis-and-allergies-connection/
Pierce-Fisher: http://www.yalescientific.org/2017/01/eczema-patients-have-a-unique-microbiome/
Kulthanan et al: 2011 https://synapse.koreamed.org/DOIx.php?id=10.5415/apallergy.2011.1.2.80
Lio and Lal: https://nationaleczema.org/leaky-gut/
Shobaili et al, 2016: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4791162/
Zheng et al 2016: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0166026
https://www.eczemacompany.com/what-is-wet-wrap-therapy-for-eczema/